- Latest news▼
-
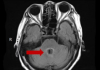
18:00, April 18 Daily Mail: Elderly woman in China gets infected with brain-eating amoeba
-
14:19, April 18 Obesity: exercising before breakfast helps you lose weight faster

-
10:42, April 18 The Conversation: childhood trauma can cause pathological hoarding

-
08:37, April 18 Daily Mail: Satiating food reduces cravings for sweets, nutritionist says

-
18:22, April 17 First Armenian-German Conference entitled “Heart Failure Spring School”

-
08:38, April 17 Why do kids usually recover from COVID-19 more easily than adults?

-
14:37, April 16 Daily Mail: intermittent fasting is not suitable for children and women before their periods

-
16:41, April 15 Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk

-
15:04, April 15 305 cases of measles recorded in Armenia so far in 2024

-
14:38, April 15 Food and Environmental Virology: tea contributes to effective coronavirus control

-
12:41, April 15 Daily Mail: vitamin A, B3 and E supplements can be dangerous

-
10:56, April 15 Diabetes Care: evening physical activity is good for the heart

-
08:27, April 15 Women are more susceptible to blood loss and death during bypass surgery than men, researchers say

-
18:42, April 13 WHO: Nigeria pioneers revolutionary meningitis vaccine

-
16:43, April 13 One-third of women experience menstruation-related migraines, most often during premenopause - study

All materials
Circadian dysfunction may ID preclinical Alzheimer's

Disruptions in rest-activity cycling occur before cognitive changes emerge and may be a biomarker of preclinical Alzheimer's disease (AD), an observational study suggested.
Amyloid plaque pathology, assessed by cerebrospinal fluid (CSF) biomarkers or positron emission tomography (PET) amyloid imaging, was associated with disturbances in rest-activity patterns in cognitively normal adults even after accounting for effects of aging and sex, reported Yo-El S. Ju, MD, of Washington University School of Medicine in St. Louis, and colleagues online in JAMA Neurology.
"We found that fragmentation of the circadian rhythm -- meaning when someone had frequent short periods of rest or sleep during the day, and frequent brief periods of activity at night -- was associated with preclinical Alzheimer's disease," Ju told MedPage Today.
This is the first study that shows deterioration of circadian rhythms occurs before any cognitive symptoms in AD, she added.
"This paper presents novel data that focuses specifically on how the misalignment of the circadian system may contribute to dysfunctional brain processes that underpin dementia, particularly Alzheimer's disease," added Sharon Naismith, DPsych, of the University of Sydney in Australia, who was not involved in the study.
The role of the circadian system in diseases like dementia is relatively underexplored, Naismith said: "With mounting evidence in this field, we may now begin to consider clinical trials of pharmacological and non-pharmacological treatments targeting the sleep-wake system and evaluating their capacity to delay the onset or slow the progression of Alzheimer's disease."
For this study, researchers studied 189 cognitively normal community volunteers from the Knight Alzheimer's Disease Research Center at Washington University from 2010 to 2012. Participants were mostly women (64%), about 67 years old on average, and highly educated.
The volunteers wore a wrist-mounted actigraph to track rest-activity data for 7 to 14 days at home and completed a sleep diary each morning.
Researchers used three different methods to analyze actigraphy data: nonparametric analysis based on raw activity counts, cosinor analysis, and empirical mode decomposition. In the nonparametric analysis, intradaily variability (IV) represented how consolidated the rest-activity rhythm was in each 24-hour period; the higher the IV, the more fragmented the rest-activity pattern.
The investigators assessed preclinical AD by longitudinal clinical assessment, amyloid imaging with Pittsburgh Compound B (PiB) PET scans, and CSF amyloid β-42 (Aβ42). They included data collected from 3 years before to 6 months after actigraphy.
PiB imaging was performed in 142 participants and 155 individuals had lumbar punctures to collect CSF. Participants were defined as amyloid negative only if all available Aβ biomarkers (both CSF Aβ42 and PiB, if available) were negative at baseline.
Of the 189 participants, 74% were amyloid negative. Those who were PiB-positive were older -- an average age of 71 years, compared to 65 years for PiB-negative individuals (P=0.001) -- and more often were APOE-ε4 carriers (65% versus 28% of PiB participants, P<0.001).
The researchers found that, in the absence of amyloid pathology, older age and male sex were associated with a significant increase in rest-activity fragmentation and decreased circadian rhythm amplitude.
After adjusting for age and sex, PiB-positive individuals had more circadian fragmentation (mean 0.875) than PiB-negative participants (mean 0.804; P=0.05).
Similarly, increasing CSF phosphorylated-tau (pTau) to Aβ42 ratio (β =0.231; P=0.008), indicating more AD pathology, was associated with increasing rest-activity fragmentation.
"Altogether, our data suggest that aging and preclinical AD pathology have separate and additive negative effects on circadian rhythm fragmentation," the researchers wrote.
The researchers also found a significant correlation between number of naps participants took and circadian fragmentation, implying that disrupted daytime rest-activity patterns might be a sign of presymptomatic AD.
Of the several circadian endpoints studied, the one that was consistently most sensitive to both aging and AD pathology was the nonparametric IV index. "Our finding that IV correlates with increasing pTau to Aβ42 ratio suggests the IV might warrant further investigation as a noninvasive biomarker of disease progression in preclinical AD," they observed.
The authors listed several limitations to their research. They did not have information about medications and comorbidities, especially sleep apnea. Age- or sex-related circadian changes in the amyloid-negative group might have been caused by non-amyloid pathologies, they added. And non-circadian factors, like voluntary exercise, might have influenced rest-activity measurements.
"Replication using other circadian parameters (such as core body temperature) could be considered to confirm our findings," they wrote.
Follow NEWS.am Medicine on Facebook and Twitter
- Video
- Event calendar
- Archive
- Most read
month
week
day
- Pediatrics: Hypoglossal nerve stimulation implant helps with sleep apnea 1343
- Health minister: Simulation educational center will be created, assisted reproductive technology capacity will increase in Armenia 1302
- WHO: Nigeria pioneers revolutionary meningitis vaccine 1153
- One-third of women experience menstruation-related migraines, most often during premenopause - study 1122
- Women are more susceptible to blood loss and death during bypass surgery than men, researchers say 830
- Food and Environmental Virology: tea contributes to effective coronavirus control 814
- Daily Mail: vitamin A, B3 and E supplements can be dangerous 812
- Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk 778
- 305 cases of measles recorded in Armenia so far in 2024 775
- Diabetes Care: evening physical activity is good for the heart 764
- Daily Mail: intermittent fasting is not suitable for children and women before their periods 591
- First Armenian-German Conference entitled “Heart Failure Spring School” 378
- Why do kids usually recover from COVID-19 more easily than adults? 190
- Daily Mail: Satiating food reduces cravings for sweets, nutritionist says 147
- The Conversation: childhood trauma can cause pathological hoarding 142
- Find us on Facebook
- Poll





