- Latest news▼
-
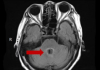
18:00, April 18 Daily Mail: Elderly woman in China gets infected with brain-eating amoeba
-
14:19, April 18 Obesity: exercising before breakfast helps you lose weight faster

-
10:42, April 18 The Conversation: childhood trauma can cause pathological hoarding

-
08:37, April 18 Daily Mail: Satiating food reduces cravings for sweets, nutritionist says

-
18:22, April 17 First Armenian-German Conference entitled “Heart Failure Spring School”

-
08:38, April 17 Why do kids usually recover from COVID-19 more easily than adults?

-
14:37, April 16 Daily Mail: intermittent fasting is not suitable for children and women before their periods

-
16:41, April 15 Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk

-
15:04, April 15 305 cases of measles recorded in Armenia so far in 2024

-
14:38, April 15 Food and Environmental Virology: tea contributes to effective coronavirus control

-
12:41, April 15 Daily Mail: vitamin A, B3 and E supplements can be dangerous

-
10:56, April 15 Diabetes Care: evening physical activity is good for the heart

-
08:27, April 15 Women are more susceptible to blood loss and death during bypass surgery than men, researchers say

-
18:42, April 13 WHO: Nigeria pioneers revolutionary meningitis vaccine

-
16:43, April 13 One-third of women experience menstruation-related migraines, most often during premenopause - study

All materials
The truth about maternal death

Women die in childbirth at alarming rates. Maternal death is an excellent example of what the famous economist and philosopher Amartya Sen calls a "remediable injustice" —a condition that is fundamentally unfair and within our capacity to change.
Access to health services is better in more affluent, developed countries, so women die of pregnancy and childbirth-related complications at much lower rates than their counterparts in developing countries.
Better access to health services and skilled practitioners —nurses, midwives, medical doctors —is one of the keys to improving maternal mortality ratios in the developing world.
The Maternal Mortality Ratio (MMR) indicates the number of maternal deaths that occur for every 100,000 live births. In 2015, the world average was 216.
The highest MMRs are found in Sub-Saharan Africa (547) and in low-income countries (496). Conversely, the lowest rates of maternal death are found in high-income countries (10), the European Union (eight) and North America (12).
These numbers reveal much about the disparities that cause high rates of maternal death in poor countries and low rates in affluent countries. Resources are scarce in developing countries, and those that are available in the form of medical expertise, facilities and supplies are distributed unevenly.
According to the World Health Organization, the leading causes of maternal death include "haemorrhage, hypertension, infections, and indirect causes, mostly due to interaction between pre-existing medical conditions and pregnancy."
Most of these causes are treatable with simple procedures and medicines. Most maternal deaths are preventable if women have access to skilled providers and health clinics during pregnancy, childbirth and in the immediate post-partum period.
But the truth about maternal death is not that simple. While it's true that better access to health care before, during and after childbirth will reduce incidents of maternal death, there are other, more complex factors to consider.
Barriers to access to health services go beyond the lack of hospitals and doctors to implicate social and cultural dynamics. In other words, women struggle to access available resources due to the realities of poverty, racial discrimination, gender inequality and the criminalization of abortion.
Furthermore, women are vulnerable to complicated pregnancies through the practices of child marriage (and adolescent pregnancy), high fertility rates (which increases the potential for obstructed labour), patriarchal customs that make women's health, nutrition and education unimportant and policies that fail to respect human rights.
Unfortunately, this is not the case in North America, where MMRs have increased in recent years. In Canada, maternal death rates went from six in 1990 to 12 in 2010, likely due to an increase in caesarean sections, IVF births, older mothers and other health conditions.
The crisis in maternal health is the focus of broad global campaigns and detailed targeted initiatives. Much of this focus is devoted to generating increased attention and resources for maternal health.
However, global agencies and individual countries must do more to address the complex contextual factors that undermine maternal health.
Maternal death rates will only continue to decline if there are broad societal changes for all women. Governments play a leading role in perpetuating maternal death and will have to assume greater responsibility to reduce it.
Follow NEWS.am Medicine on Facebook and Twitter
- Video
- Event calendar
- Archive
- Most read
month
week
day
- Pediatrics: Hypoglossal nerve stimulation implant helps with sleep apnea 1356
- Health minister: Simulation educational center will be created, assisted reproductive technology capacity will increase in Armenia 1311
- WHO: Nigeria pioneers revolutionary meningitis vaccine 1164
- One-third of women experience menstruation-related migraines, most often during premenopause - study 1132
- Women are more susceptible to blood loss and death during bypass surgery than men, researchers say 907
- Daily Mail: vitamin A, B3 and E supplements can be dangerous 886
- Food and Environmental Virology: tea contributes to effective coronavirus control 886
- Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk 855
- 305 cases of measles recorded in Armenia so far in 2024 849
- Diabetes Care: evening physical activity is good for the heart 839
- Daily Mail: intermittent fasting is not suitable for children and women before their periods 664
- First Armenian-German Conference entitled “Heart Failure Spring School” 455
- Why do kids usually recover from COVID-19 more easily than adults? 318
- Obesity: exercising before breakfast helps you lose weight faster 301
- The Conversation: childhood trauma can cause pathological hoarding 297
- Find us on Facebook
- Poll





