- Latest news▼
-
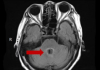
18:00, April 18 Daily Mail: Elderly woman in China gets infected with brain-eating amoeba
-
14:19, April 18 Obesity: exercising before breakfast helps you lose weight faster

-
10:42, April 18 The Conversation: childhood trauma can cause pathological hoarding

-
08:37, April 18 Daily Mail: Satiating food reduces cravings for sweets, nutritionist says

-
18:22, April 17 First Armenian-German Conference entitled “Heart Failure Spring School”

-
08:38, April 17 Why do kids usually recover from COVID-19 more easily than adults?

-
14:37, April 16 Daily Mail: intermittent fasting is not suitable for children and women before their periods

-
16:41, April 15 Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk

-
15:04, April 15 305 cases of measles recorded in Armenia so far in 2024

-
14:38, April 15 Food and Environmental Virology: tea contributes to effective coronavirus control

-
12:41, April 15 Daily Mail: vitamin A, B3 and E supplements can be dangerous

-
10:56, April 15 Diabetes Care: evening physical activity is good for the heart

-
08:27, April 15 Women are more susceptible to blood loss and death during bypass surgery than men, researchers say

-
18:42, April 13 WHO: Nigeria pioneers revolutionary meningitis vaccine

-
16:43, April 13 One-third of women experience menstruation-related migraines, most often during premenopause - study

All materials
Genome-wide meta-analysis implicates mediators of hair follicle development and morphogenesis in risk for severe acne

Acne vulgaris is a highly heritable common, chronic inflammatory disease of the skin for which five genetic risk loci have so far been identified. Here, we perform a genome-wide association study of 3823 cases and 16,144 controls followed by meta-analysis with summary statistics from a previous study, with a total sample size of 26,722. We identify 20 independent association signals at 15 risk loci, 12 of which have not been previously implicated in the disease. Likely causal variants disrupt the coding region of WNT10A and a P63 transcription factor binding site in SEMA4B. Risk alleles at the 1q25 locus are associated with increased expression of LAMC2, in which biallelic loss-of-function mutations cause the blistering skin disease epidermolysis bullosa. These findings indicate that variation affecting the structure and maintenance of the skin, in particular the pilosebaceous unit, is a critical aspect of the genetic predisposition to severe acne.
Acne vulgaris is an inflammatory disease of the skin, primarily affecting the face, chest and back. The biological mechanisms that lead to lesion development are poorly understood, but involve a complex interplay between sebum production, follicular keratinisation, inflammation, and colonisation of pilosebaceous follicles by Propionibacterium acnes1. The characteristic inflammatory papules, pustules and nodules typically first develop during puberty, may persist for decades and leave disfiguring scars in up to 20% of patients. Acne can have severe emotional and psychological consequences and has been associated with depression, unemployment, suicidal ideation and suicide itself1. Severe acne is typically treated with topical and systemic agents that suppress the microbiome repertoire or the activity of sebaceous glands. The treatment regimes are often ineffective and poorly tolerated, and there remains a substantial unmet medical need.
Evidence of a genetic component to acne susceptibility is well established2 and previous genome-wide association studies (GWAS) of severe acne have identified three genomic loci harbouring alleles that are associated with the disease in the European population3, and two in the Han Chinese population4. These loci have provided insight into the biological mechanisms that underlie disease pathogenesis, including a potential role for components of the TGFβ pathway.
In the current study, we further delineate the genetic susceptibility of severe acne through the identification of genetic variation at 15 genomic loci that contribute to disease risk. Investigation of the consequence of the associated alleles at these loci indicates that the contribution to acne susceptibility may be, at least in part, mediated through variation in the structure and maintenance of the pilosebaceous unit in the skin.
Genome-wide association study and meta-analysis
To investigate the genetic basis of acne we have performed a GWAS of 3823 severe acne cases, recruited through a network of hospital-based dermatologists within the United Kingdom, and 16,144 unselected population controls. Following quality control and genome-wide imputation we tested more than 7.4 million SNPs for association with acne. At the three loci (1q41, 5q11.2 and 11q13.1) harbouring acne-associated alleles in an independent UK acne study population3, we observed strong evidence of association with a consistent direction and magnitude of effect as was previously reported . However, we did not replicate the associations at 1q24.2 or 11p11.2 described in the Han Chinese population4, highlighting potential trans-ethnic differences in the genetic contributors to acne susceptibility.
Full article: Nature Communications
Follow NEWS.am Medicine on Facebook and Twitter
- Video
- Event calendar
- Archive
- Most read
month
week
day
- Pediatrics: Hypoglossal nerve stimulation implant helps with sleep apnea 1353
- Health minister: Simulation educational center will be created, assisted reproductive technology capacity will increase in Armenia 1310
- WHO: Nigeria pioneers revolutionary meningitis vaccine 1164
- One-third of women experience menstruation-related migraines, most often during premenopause - study 1132
- Women are more susceptible to blood loss and death during bypass surgery than men, researchers say 883
- Daily Mail: vitamin A, B3 and E supplements can be dangerous 862
- Food and Environmental Virology: tea contributes to effective coronavirus control 862
- Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk 830
- 305 cases of measles recorded in Armenia so far in 2024 825
- Diabetes Care: evening physical activity is good for the heart 814
- Daily Mail: intermittent fasting is not suitable for children and women before their periods 639
- First Armenian-German Conference entitled “Heart Failure Spring School” 426
- Why do kids usually recover from COVID-19 more easily than adults? 280
- The Conversation: childhood trauma can cause pathological hoarding 257
- Obesity: exercising before breakfast helps you lose weight faster 253
- Find us on Facebook
- Poll





