- Latest news▼
-
10:23, April 19 JAMA Oncology: Urine test can help rule out high-grade prostate cancer with almost 100% accuracy, study shows

-
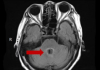
18:00, April 18 Daily Mail: Elderly woman in China gets infected with brain-eating amoeba
-
14:19, April 18 Obesity: exercising before breakfast helps you lose weight faster

-
10:42, April 18 The Conversation: childhood trauma can cause pathological hoarding

-
08:37, April 18 Daily Mail: Satiating food reduces cravings for sweets, nutritionist says

-
18:22, April 17 First Armenian-German Conference entitled “Heart Failure Spring School”

-
08:38, April 17 Why do kids usually recover from COVID-19 more easily than adults?

-
14:37, April 16 Daily Mail: intermittent fasting is not suitable for children and women before their periods

-
16:41, April 15 Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk

-
15:04, April 15 305 cases of measles recorded in Armenia so far in 2024

-
14:38, April 15 Food and Environmental Virology: tea contributes to effective coronavirus control

-
12:41, April 15 Daily Mail: vitamin A, B3 and E supplements can be dangerous

-
10:56, April 15 Diabetes Care: evening physical activity is good for the heart

-
08:27, April 15 Women are more susceptible to blood loss and death during bypass surgery than men, researchers say

-
18:42, April 13 WHO: Nigeria pioneers revolutionary meningitis vaccine

All materials
Global patterns in excess body weight and the associated cancer burden

Abstract
The prevalence of excess body weight and the associated cancer burden have been rising over the past several decades globally. Between 1975 and 2016, the prevalence of excess body weight in adults—defined as a body mass index (BMI) ≥ 25 kg/m2—increased from nearly 21% in men and 24% in women to approximately 40% in both sexes. Notably, the prevalence of obesity (BMI ≥ 30 kg/m2) quadrupled in men, from 3% to 12%, and more than doubled in women, from 7% to 16%. This change, combined with population growth, resulted in a more than 6‐fold increase in the number of obese adults, from 100 to 671 million. The largest absolute increase in obesity occurred among men and boys in high‐income Western countries and among women and girls in Central Asia, the Middle East, and North Africa.
The simultaneous rise in excess body weight in almost all countries is thought to be driven largely by changes in the global food system, which promotes energy‐dense, nutrient‐poor foods, alongside reduced opportunities for physical activity. In 2012, excess body weight accounted for approximately 3.9% of all cancers (544,300 cases) with proportion varying from less than 1% in low‐income countries to 7% or 8% in some high‐income Western countries and in Middle Eastern and Northern African countries. The attributable burden by sex was higher for women (368,500 cases) than for men (175,800 cases).
Given the pandemic proportion of excess body weight in high‐income countries and the increasing prevalence in low‐ and middle‐income countries, the global cancer burden attributable to this condition is likely to increase in the future. There is emerging consensus on opportunities for obesity control through the multisectoral coordinated implementation of core policy actions to promote an environment conducive to a healthy diet and active living. The rapid increase in both the prevalence of excess body weight and the associated cancer burden highlights the need for a rejuvenated focus on identifying, implementing, and evaluating interventions to prevent and control excess body weight.
Introduction
Overweight and obesity, collectively referred to as “excess body weight,” are defined as abnormal or excessive fat accumulation that causes many chronic diseases and reduces life expectancy. The prevalence of excess body weight has been increasing worldwide since the 1970s, and in 2016, approximately 40% of adults and 18% of children (ages 5‐19 years) had excess body weight, equating to almost 2 billion adults and 340 million children. This trend is taking a toll on health; in 2015, an estimated 4 million deaths were attributable to excess body weight. The economic impact of illness related to excess body weight is daunting, estimated at US $2.0 trillion globally in 2014. Except for a possible plateau in high‐income countries in recent years, the prevalence of excess body weight has increased rapidly in most countries across all population groups. Some of the steepest increases are in low‐ and middle‐income countries, likely as a result of the introduction of the “Western lifestyle,” consisting of energy‐dense, nutrient‐poor foods alongside reduced physical activity levels.
Excess body weight is associated with the risk of various cancers. Although the effects of excess body weight on cancer risk are modest for most cancer sites, excess body weight is highly prevalent in high‐income countries and elsewhere, leading to a substantial burden of cancers. In 2012, it was estimated at 544,300 cases, or 3.9% of all cancers worldwide,8 and this number undoubtedly will rise in the coming decades given current trends.8
In this review, we present global and regional patterns in excess body weight, drivers of the epidemic, a summary of epidemiological evidence supporting the causal link of excess body weight to cancer risk, and the attributable cancer burden. Core policy actions to prevent and control excess body weight also are discussed.
Defining Excess Body Weight
Body mass index (BMI), defined as body mass in kilograms divided by the square of height in meters (kg/m2), is the most commonly used anthropometric measure to approximate overall body fatness for the purposes of classifying and reporting overweight and obesity.9 The World Health Organization (WHO) classifies adults with a BMI below 18.5 kg/m2 as “underweight” and between 18.5 and 24.9 kg/m2 as “normal.”1 Above the normal range, there are conventional gradings for “overweight” (25‐29.9 kg/m2) and “obesity” (30 kg/m2 or greater). Obesity can be further divided into class 1 (30.0‐34.9 kg/m2), class 2 (35.0‐39.9 kg/m2), and class 3 (40 kg/m2 or greater). Among children, overweight and obesity are defined not by absolute BMI cutoff points but relative to a historical healthy‐weight group.1, 10 The WHO provides different sets of standards for school‐aged children (ages 5‐19 years) and children younger than 5 year.
Full article: СА
Follow NEWS.am Medicine on Facebook and Twitter
- Video
- Event calendar
- Archive
- Most read
month
week
day
- Pediatrics: Hypoglossal nerve stimulation implant helps with sleep apnea 1365
- WHO: Nigeria pioneers revolutionary meningitis vaccine 1171
- One-third of women experience menstruation-related migraines, most often during premenopause - study 1137
- Women are more susceptible to blood loss and death during bypass surgery than men, researchers say 953
- Food and Environmental Virology: tea contributes to effective coronavirus control 939
- Daily Mail: vitamin A, B3 and E supplements can be dangerous 938
- Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk 910
- 305 cases of measles recorded in Armenia so far in 2024 902
- Diabetes Care: evening physical activity is good for the heart 892
- Daily Mail: intermittent fasting is not suitable for children and women before their periods 718
- First Armenian-German Conference entitled “Heart Failure Spring School” 508
- Why do kids usually recover from COVID-19 more easily than adults? 380
- Obesity: exercising before breakfast helps you lose weight faster 367
- The Conversation: childhood trauma can cause pathological hoarding 359
- Daily Mail: Satiating food reduces cravings for sweets, nutritionist says 334
- Find us on Facebook
- Poll





