Virus fished from pond cures man’s deadly antibiotic-resistant infection
 12:33 22 March, 2018
12:33 22 March, 2018In 2012, a 76-year-old Connecticut doctor had surgery to repair a life-threatening bulge in his aortic arch—the hulking bend that hooks the massive artery around the heart, routing oxygenated blood both upward and downward. Surgeons successfully used a synthetic graft to shore up the vital conduit. But soon after, a tenacious film of drug-resistant Pseudomonas aeruginosa bacteria formed on the graft.
The doctor spent the next four years battling the infection, slipping in and out of the hospital. His surgeons and doctors at Yale deemed him too high risk for another operation and put him on mega-doses of antibiotics, prescribed indefinitely. The drugs couldn’t clear the infection, they merely knocked it back enough to keep it from killing him. But the chronic inflammation that ensued took its own toll. His team of doctors started to worry his immune system was chipping away at his aorta. With a bleak outlook, the man agreed in 2016 to an experimental treatment: a virus that researchers had fished out of a nearby pond.
The viral gamble paid off. The infection cleared and he went off antibiotics, according to a case study published recently by the Yale researchers and doctors in the journal of Evolution, Medicine, and Public Health.
Phages for the ages
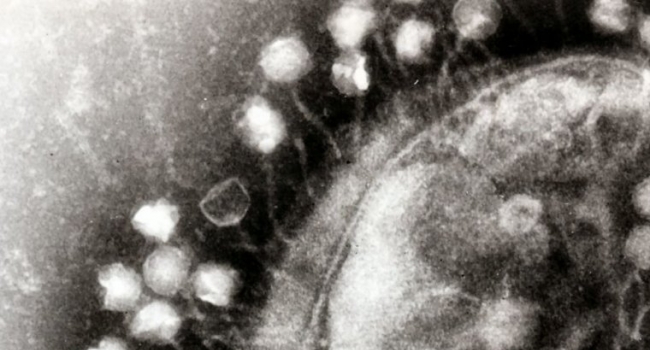
The case is a clinical win for using viruses when antibiotics fail to kill bacteria. It’s an idea that has been around for decades. Viruses that exclusively infect and kill bacteria—called “bacteriophages” or just “phages”—have been used in former Soviet republics and some parts of Eastern Europe for nearly a century. Phages kill in the same way as many viruses; a phage infects a host cell, usurps its cellular machinery to make copies of itself, then the clone army bursts out, destroying the host cell in the process. And there are plenty of phages to harness for potential therapies. In water samples, for instance, some researchers have estimated that there are 10 phages for every bacterial/archaeal cell. To put that in perspective, the open ocean is estimated to contain 1.2 × 1029 bacterial and archaeal cells.
Never-before-seen viruses that can kill bacteria stream from women’s bladders
But in Westernized countries, phage therapy has largely been passed over by researchers, given the success of antibiotics. As such, phages have failed to garner the needed research attention to establish their safety and efficacy. That’s changing now, albeit slowly, with the rise of antibiotic-resistant bacteria.
But this pond phage isn’t your garden-variety microbial marauder. The phage—dubbed OMKO1—has the unique ability to force surviving drug-resistant bacteria into ditching their drug resistance. This is critical. One of the main arguments against turning to phage therapy is that bacteria can readily evolve resistance to them. Researchers have plenty of evidence of this. Thus, some researchers fear that any effective phage therapy is destined to the same impotent fate as many of our once powerful antibiotics.
But, if phages can kill bacteria and make survivors evolve to be vulnerable to drugs, then a one-two punch of phage and drugs could knock out any infection, resistant or not. In other words, “phage such as OMKO1 that appear to force a clinically relevant trade-off may present an effective solution to the inevitable evolution of resistance by pathogenic bacteria,” the Yale researchers conclude.
Viral KO
Those researchers, led by surgeon Deepak Narayan and ecology and evolutionary biologist Paul Turner, wanted exactly this type of phage for the sick doctor. Luckily, Turner had been surveying phages from environmental samples that could strong-arm bacteria into a deadly genetic trade-off.
Turner and his lab had collected phages from sewage, soil, lakes, rivers, streams, and compost. They found 42 that could infect P. aeruginosa, an abundant opportunistic pathogen often found to be resistant to antibiotics. The researchers were motivated to go after this particular pathogen because it is “poised to become a common [pan-drug-resistant] disease problem,” Turner and his colleagues wrote in 2016. That is, they suspect it will become resistant to all potential antibiotic treatments in the foreseeable future.
Turner and his team hypothesized that they could wipe the floor with resistant P. aeruginosa if they matched the phage to the type of drug resistance the bacteria carry. Phages, like all killer viruses, need to be able to recognize and grab onto a potential host cell before it can invade and kill. Influenza viruses famously do this by latching onto sialic acids that hang on the outside of human cells in the respiratory tract.
Conveniently, P. aeruginosa thwarts many antibiotics using a bit of machinery called an efflux pump. This molecular device works a lot like a sump pump, creating a pore in the cell through which it actively pumps out certain antibiotics before they can cause cellular damage. As such, the pump is situated at the outer membrane—where phages can latch on to it.
In their survey, Turner and company found one phage that infected P. aeruginosa by grabbing on to part of this pump, a part called the outer membrane porin M. The phage was collected from Dodge Pond, about 65km east of Yale. The researchers dubbed it OMKO1 or outer-membrane-porin M knockout dependent phage #1.
If the deadly bacteria have the pump, the phage can grab hold and kill them. If the bacteria lack the pump or have a mutant, broken version, that means that phage can’t get in and kill—but standard antibiotics can.
Saving the doctor
In early lab tests, published in Scientific Reports in 2016, Turner and his lab showed that as P. aeruginosa evolved resistance to OMKO1, it became more susceptible to antibiotic treatments. To verify that this phage could one day be clinically useful, they tested it out on several P. aeruginosa strains that Yale colleagues had isolated from patients—including one who had a chronic infection on an aortic arch graft.
As Turner and his lab carried out their work, the doctor’s health continued to slip. Doctors and researchers made the bold decision to try out the phage. Turner’s lab collected bacteria-laden discharge from a fistula that formed in the doctor’s chest and mixed it with phage. The pond virus killed off most of the bacteria and re-sensitized the survivors to antibiotics. With such promising lab results, the team got an emergency investigational new drug approval from the Food and Drug Administration to treat the sick doctor with their pond phage.
With the doctor’s aorta seemingly disintegrating, Narayan and Turner’s teams injected a high dose of purified OMKO1 in combination with the antibiotic ceftazidime directly into the fistula in his chest.
The next day, the doctor had stable vital signs and had no complaints. He was subsequently released from the hospital. Things were looking up until four weeks later, when his chest wound started bleeding. Doctors had no choice but to perform emergency surgery. With his chest open, the surgeons found that a bone fragment from his sternum had broken off and pierced his aorta. But what they didn’t find was any evidence of a P. aeruginosa infection. The surgeons repaired damage and replaced the aortic graft. Shortly after, they took him off antibiotics and he has been off them ever since.
The researchers concluded that the phage was critical for ridding the doctor of his deadly infection. “Eventual controlled trials examining phage application as adjunctives may reveal improved clinical outcomes in cases of recalcitrant infection,” they wrote.
For now, they conclude, “the current case study indicates the fortuitous possibility for a single phage to apparently resolve the bacterial infection, where pre-treatment understanding of the evolutionary mechanism… underlying bacterial resistance informed the choice of phage used in experimental therapy.”