- Latest news▼
-
19:41, April 25 Children’s Hospital Los Angeles and International Center of Professional Development Allergy/Immunology Conference

-
17:31, April 25 JAMA: patient grew long, curly eyelashes because of chemotherapy

-
11:08, April 25 Mpox epidemic declared in Republic of the Congo

-
08:31, April 25 OU: quitting smoking 4 times more likely to cure laryngeal cancer

-
01:20, April 25 Paralyzed man in China writes hieroglyphs using neural implants placed in his brain

-
15:11, April 24 Zombie deer disease possibly linked to hunters’ deaths

-
12:27, April 23 Appetite: Scientists found out the secret to the appeal of large portions of fast food

-
10:33, April 23 Scientists test new approach to fighting viruses

-
08:38, April 23 Ketamine may help with postpartum depression

-
22:12, April 22 Unhealthy amount of sugar found in baby food products of a well-known brand

-
19:41, April 22 Air pollution puts health of more than 1.6 billion workers globally at risk

-
17:25, April 22 Scientists found baked goods and lack of sleep to be more dangerous than alcohol

-
16:02, April 22 342 cases of measles recorded in Armenia so far in 2024

-
15:29, April 22 BrainStimulation: electrical brain stimulation alleviates anxiety and depression in the elderly

-
08:27, April 22 Cognitively stimulating jobs in midlife could lower dementia risk in old age, study finds

All materials
Most popular form of IVF given to thousands of couples is ineffective, scientists say
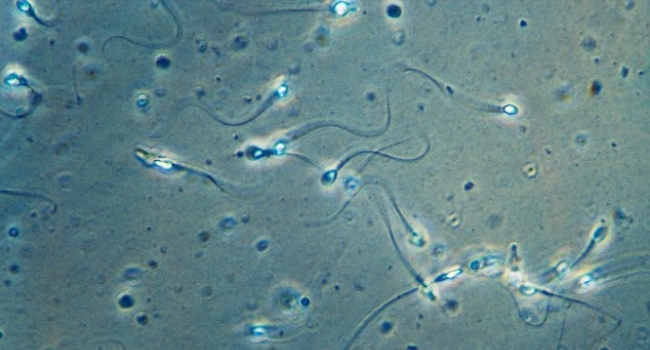
The most popular form of IVF is 'ineffective and costly' and may actually reduce a woman's chances of getting pregnant, a leading fertility expert has warned.
Professor Hans Evers, editor-in-chief of the Human Reproduction journal, criticised IVF clinics for handing out an expensive IVF add-on treatment to couples who will not benefit from it.
Doctors are guilty of over-estimating the effect of intracytoplasmic sperm injection (ICSI) - which was used by 455,000 couples in 2010 - he said.
ICSI is a treatment where a single sperm is injected into the egg - and was developed for use when the man has been diagnosed with infertility and there is a severe problem with his sperm.
Only 30 to 40 per cent of couples' problems are caused by severe male infertility, so scientists say no more than 40 per cent should have ICSI.
But more than half of British couples undergoing IVF have the additional treatment - which typically costs between £1,000 and £1,500 per cycle.
It usually adds around a third on top of the cost of IVF, raising fears some clinics may be promoting it to boost profits.
Professor Evers said inappropriate treatments should be 'weeded out' and clinicians needed to stop 'playing Santa Claus and doling out nicely wrapped presents of unnecessary, ineffective and costly care.'
When given to couples where male infertility isn't the problem - it could even lower their chances of conceiving, he warned.
He said: 'The majority of the patients who will get pregnant with ICSI will also do so with IVF.'
Studies show ICSI results in fewer live births than IVF when used for couples where male infertility is not the problem.
Professor Evers continued: 'Intending to improve their patients' pregnancy probability by preventing fertilisation failure, well meaning doctors actually decrease their chances.
'This has to stop. We have pledged to do no harm.'
Professor Evers said in 2010 there were 220,000 IVF procedures but more than 455,000 ICSI (intracytoplasmic sperm injection) in the world.
In the UK, 55.3 per cent of UK couples undergoing fertility treatment in 2010 had ICSI – a rate of 1.2 treatments for every one case of IVF.
Professor Evers said the rate showed 'some overuse', compared to the ideal figure of 0.66 ICSI treatments for every one of IVF.
The figure is higher than that of Ireland, where it is 0.8, and Scandinavian countries where it ranges from 0.8 to 1.1. But it is far below other EU countries like Spain, where it is 9.0, and Poland, where it is 25.4.
In the Middle East it is as high as 60.3, with nearly all couples undergoing fertility treatment having ICSI.
Commenting on the research, Professor Geeta Nargund, medical director of Create Fertility, said it was 'unacceptable' for clinics to increase costs to patients by giving them unnecessary treatments.
She told the Mail: 'ICSI is also an invasive technique which is not without risk. Where possible we should be using more natural and less invasive methods for conception.
'We have a duty and an obligation to reduce invasive techniques, to reduce the cost to patients, to make treatment as natural and as safe as possible.'
The figures relate to 2010 – the most recent year available - and are based on data from nearly 2,500 clinics in between 58 and 61 countries, from 2008 to 2010.
During the three-year period, nearly 4.5million treatment cycles were carried out, resulting in around 1,144,858 babies being born around the world.
Previous research has suggested ICSI treatment creates a 'sky high' chance of having a baby with serious abnormalities.
The study of 300,000 births found one child in ten born following ICSI had a defect - twice the level of the general population - but that standard IVF has no extra risks compared with natural births.
These include a cleft palate, heart and lung conditions, cerebral palsy and blood disorders.
Professor Evers' comments come just a week after fertility clinic regulator the Human Fertilisation and Embryology Authority (HFEA) raised concerns patients were being confused by 'extras' offered by clinic and often paid out without being sure they needed them.
Chairwoman Sally Cheshire said: 'Patients are often not sure whether they need the additional treatments, but worry that they could regret not making every attempt they can to get pregnant.'
Her comments followed a series of interviews in The Independent with fertility experts who criticised the use of IVF 'extras' such as immune system-suppressing drugs, pre-implantation testing and time-lapse photography.
They warned that there was little or no evidence these techniques worked and that some may even be harmful.
Follow NEWS.am Medicine on Facebook and Twitter
- Video
- Event calendar
- Children’s Hospital Los Angeles and International Center of Professional Development Allergy/Immunology Conference
- First Armenian-German Conference entitled “Heart Failure Spring School”
- Allogeneic bone marrow transplant in case of hematological malignancy performed in Armenia for first time
All materials
- Archive
- Most read
month
week
day
- JAMA Oncology: Urine test can help rule out high-grade prostate cancer with almost 100% accuracy, study shows 1312
- Scientists grow human mini-lungs in lab 1178
- Next pandemic likely to be triggered by flu - scientists 963
- Scientists found baked goods and lack of sleep to be more dangerous than alcohol 940
- 342 cases of measles recorded in Armenia so far in 2024 896
- Scientists develop new method to safely stimulate immune cells to fight cancer 786
- Cognitively stimulating jobs in midlife could lower dementia risk in old age, study finds 784
- Blood test can determine who is at risk of developing multiple sclerosis - scientists 782
- BrainStimulation: electrical brain stimulation alleviates anxiety and depression in the elderly 722
- Ketamine may help with postpartum depression 676
- Unhealthy amount of sugar found in baby food products of a well-known brand 675
- Appetite: Scientists found out the secret to the appeal of large portions of fast food 666
- Air pollution puts health of more than 1.6 billion workers globally at risk 666
- Scientists test new approach to fighting viruses 653
- Zombie deer disease possibly linked to hunters’ deaths 567
- Find us on Facebook
- Poll





