- Latest news▼
-
12:16, April 19 Scientists grow human mini-lungs in lab

-
10:23, April 19 JAMA Oncology: Urine test can help rule out high-grade prostate cancer with almost 100% accuracy, study shows

-
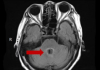
18:00, April 18 Daily Mail: Elderly woman in China gets infected with brain-eating amoeba
-
14:19, April 18 Obesity: exercising before breakfast helps you lose weight faster

-
10:42, April 18 The Conversation: childhood trauma can cause pathological hoarding

-
08:37, April 18 Daily Mail: Satiating food reduces cravings for sweets, nutritionist says

-
18:22, April 17 First Armenian-German Conference entitled “Heart Failure Spring School”

-
08:38, April 17 Why do kids usually recover from COVID-19 more easily than adults?

-
14:37, April 16 Daily Mail: intermittent fasting is not suitable for children and women before their periods

-
16:41, April 15 Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk

-
15:04, April 15 305 cases of measles recorded in Armenia so far in 2024

-
14:38, April 15 Food and Environmental Virology: tea contributes to effective coronavirus control

-
12:41, April 15 Daily Mail: vitamin A, B3 and E supplements can be dangerous

-
10:56, April 15 Diabetes Care: evening physical activity is good for the heart

-
08:27, April 15 Women are more susceptible to blood loss and death during bypass surgery than men, researchers say

All materials
Baby lived after his mother’s waters broke at 16th week

Sheila Bhatti’s GP put the damp patches down to embarrassing accidents. At four months pregnant, she accepted it was just something she’d have to put up with as part of her condition.
It was only when she went for her 20-week scan four weeks later that the horrifying truth emerged – her waters had broken just 16 weeks into her pregnancy.
“At first it was just tiny amounts, but a few days later I woke up in the night to find my pyjama bottoms were wet through,” recalls Sheila.
Her GP assured her she had probably just wet herself or was suffering from increased vaginal discharge, which is normal in pregnancy.
The 24-year-old mum-to-be left the surgery without an examination which would have revealed her waters had broken and were slowly leaking – putting her baby ’s life at terrible risk.
It was only when she went for her scan at Hillingdon Hospital in Uxbridge, Middlesex, that she realised something was seriously wrong. “The midwife looked concerned,” says Sheila, who works as a customer agent at Cineworld. “There was a heartbeat, but she couldn’t see the baby. Then she told me that my waters had ruptured, and at first I was relieved because it meant I hadn’t lost my baby.”
It was only when she was taken up to triage, where a consultant explained the situation, did she understand the gravity of what had happened.
“They asked me if I had noticed any waters leaking and I told them about the damp patches,” she says.
“They said that had been my waters going and I felt so stupid. I was told I had suffered PPROM – Pre-term Premature Rupture of Membranes – which I’d never even heard of.
“The doctors told me they were certain my baby couldn’t survive to a viable gestation and that I should consider terminating there and then. I couldn’t believe it.”
There was so little amniotic fluid left around the baby medics couldn’t even do a proper scan so had no way of knowing if it was a boy or girl.
But as her baby’s heartbeat was so strong Sheila refused to end its life and was instead admitted to a ward where doctors said nature would take its course.
“I loved my baby already and I couldn’t terminate,” says Sheila. “And when my baby continued to cling on despite having been given a less than one per cent survival chance my husband Wahab agreed that where there was life there was hope.”
After a month of bed rest, during which time her blood pressure was checked every three hours and her bloods were tested for infection three times a week, the baby was almost at the 24-week mark, the age at which a premature baby is deemed viable and medics will attempt to save its life.
Sheila, from Southall, Middlesex was moved to Queen Charlotte and Chelsea Hospital where they were better equipped to deal with very premature babies.
“To me, 24 weeks was a milestone I was desperate to reach,” she says. “I knew that a baby born this early would require a lot of intervention, including mechanical ventilation and other invasive treatments, followed by a lengthy stay in a neonatal intensive care unit – but to me, it was something to aim for.”
Yet even when, against all the odds, her baby was still hanging on, doctors enquired about funeral arrangements. “I was heartbroken,” says Sheila. “I kept telling them, ‘But my baby is still alive’. They looked at me with pity, replying, ‘I think it’s very unlikely it will survive’.
“I wasn’t naïve. I knew my baby could have disabilities and other problems, but I knew that whatever difficulties it faced I would be there.”
At 24 weeks, Sheila was given steroid injections to boost her baby’s underdeveloped lungs.
“That felt like the first time my baby had actually received any help to live, rather than just being offered help to die,” she says.
Eventually, after almost two months in hospital and still no sign of labour, Sheila was sent home at 27 weeks with instructions to go back to hospital for twice-weekly check-ups. A week and a half later, her contractions started.
In the early hours of November 14, having reached 28 weeks and five days, she went straight to the labour ward at Hillingdon hospital. But there was a problem – Sheila’s cervix wasn’t opening due to an infection. She was transferred back to Queen Charlotte’s where the baby was delivered by Caesarean section, weighing just 2lb.
“It all happened so quickly,” says Sheila. “I knew at last my baby was a boy but at first, I didn’t know if he was alive. We named him Rayyan, which means ‘wise’, as he was already beating the odds of survival. He was whisked down to the neo-natal intensive care unit.”
Sheila didn’t get to see him until 5.30pm when Wahab, 29, wheeled her down to the unit. Doctors told her that although Rayyan needed help breathing, his heart was strong.
The next 48 hours would be crucial. “I was so shocked when I saw him for the first time,” she says. “He looked so tiny, like a baby bird, and his skin was translucent and covered in wires. Still I was delighted to be a mum and spent every day sitting next to his incubator, willing him to be strong.
“After a week I could hold him. The nurses placed him on my chest, skin to skin. He felt almost weightless. Like a little scrap of life.
“Just looking at him made me cry. I feared the worst – especially when we were told he had chronic lung disease. I wondered how could he possibly survive.”
Rayyan needed several blood transfusions and at four-and-a-half months, he had surgery to remove a hernia.
“I started to pray for him,” says Sheila. “I talked and sang to him. I decided I had to be positive.”
Reaching Rayyan’s due date, February 1 2016, hit Sheila hard. “I thought of the way things should have turned out.”
She turned to the internet to connect with other mothers who had suffered PPROM. “I found a group on Facebook called Little Heartbeats, run by a mother who had lost her daughter,” she says.
“She was such a support and through her group I met mothers whose children had survived PPROM and it gave me hope that my baby might too, even though nobody had heard of it happening so early in pregnancy before.”
Very slowly Rayyan started to show signs of improvement. He was putting on weight, his tiny limbs were getting stronger. Gradually he was weaned off the machines and managed to breathe independently.
At five months old, he weighed 9lb and was finally well enough to go home.
“It was the best day of my life, but I was scared too,” says Sheila. “Rayyan had been through so much in his short life. What if he relapsed?
“It was hard letting go of the safety net that surrounded us at the hospital. I checked on him several times a night, holding my own breath until I was sure he was breathing.
“But it’s fantastic to have him home with us. Now that I can push him round the park in his pram, I finally feel like a proper mum.
“We don’t know what the future holds but we’re just happy he’s alive. It may take him longer than normal to get better from childhood illnesses.
“But his whole life he’s kept proving everyone wrong – and I hope my story gives other mums hope.”
Follow NEWS.am Medicine on Facebook and Twitter
- Related News
- US woman is cured just few hours after being diagnosed with lung cancer April Boudreau, 61, of Texas, was receiving yearly CT scans after having survived cancer three times already...
- Exclusive interview: Young woman defeats stage 4 breast cancer “Some people after us will have to face the same, and they need to know that there were other people who have been through the same…
- Teen survives after car fell on his head “Juan had been riding in his friend’s car near his school when the accident occurred…
- Toddler with cancerous tumour undergoes unique surgery Doctors first assumed that the cause of the ailment is a virus…
- UK youngest baby born at 23 weeks may get in Guinness Book of Records Edie Madoc-Jones weighed 1lb 4oz…
- Video
- Event calendar
- Archive
- Most read
month
week
day
- WHO: Nigeria pioneers revolutionary meningitis vaccine 1180
- One-third of women experience menstruation-related migraines, most often during premenopause - study 1163
- Daily Mail: vitamin A, B3 and E supplements can be dangerous 1003
- Food and Environmental Virology: tea contributes to effective coronavirus control 1000
- Cell: in carriers of defective BRCA2 gene, sugar consumption increases cancer risk 972
- 305 cases of measles recorded in Armenia so far in 2024 964
- Women are more susceptible to blood loss and death during bypass surgery than men, researchers say 962
- Diabetes Care: evening physical activity is good for the heart 922
- Daily Mail: intermittent fasting is not suitable for children and women before their periods 781
- First Armenian-German Conference entitled “Heart Failure Spring School” 565
- Why do kids usually recover from COVID-19 more easily than adults? 449
- The Conversation: childhood trauma can cause pathological hoarding 447
- Obesity: exercising before breakfast helps you lose weight faster 447
- Daily Mail: Elderly woman in China gets infected with brain-eating amoeba 411
- Daily Mail: Satiating food reduces cravings for sweets, nutritionist says 408
- Find us on Facebook
- Poll





